Alzheimer’s disease (AD) is the most common form of dementia and usually begins in late middle age. In the past, it was considered a rare disorder, but now is viewed as a major public health concern that has a tremendous impact on millions of older people and their families. Dementia affects approximately 4 million Americans and is projected to affect more than 14 million by 2050. AD accounts for 50-75% of neurodegenerative dementia cases. Approximately 13% of individuals over the age of 65 are diagnosed with AD. Characteristics of AD are memory lapses/losses, confusion, emotional instability, and progressive loss of mental ability, as well as personality changes.
PET-CT in the Investigation of Dementia
The role of imaging in AD is to exclude “treatable” causes, to clarify diagnostic dilemmas, and to identify early onset cases for possible innovative therapies in clinical trials. When the cause of dementia is determined to be AD, it is best to discover it sooner, rather than later. The main benefit is that drugs are now available to treat AD and can help some people to maintain their mental abilities for months or even years.
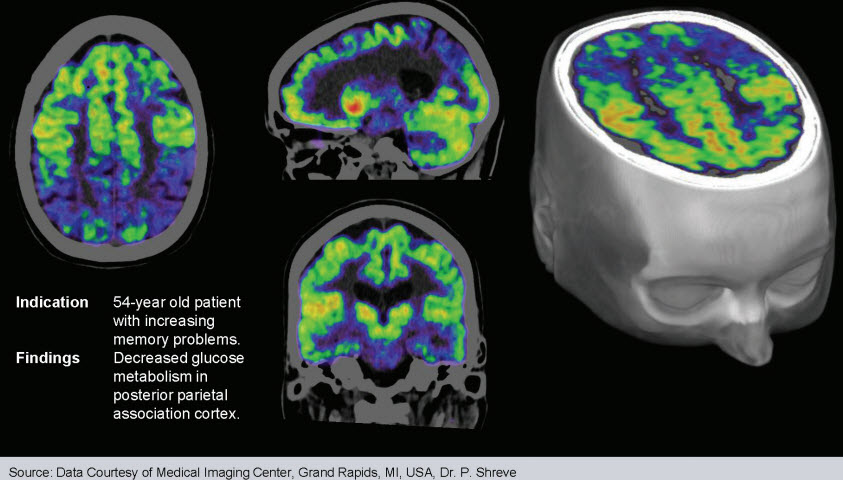
Positron emission tomography (PET) – Computer tomography (CT) is a medical imaging technique that provides a three-dimensional representation of the rates of biochemical and physiologic processes of the brain. PET-CT uses radiolabeled glucose analogue FDG to measure glucose metabolism, which indicates levels of neurosynaptic activity.
Such imaging can differentiate people with Alzheimer’s disease (AD) from those with other dementias. Alzheimer’s disease, frontotemporal dementia (FTD), multi-infarct dementia, progressive supranuclear palsy, Huntington’s disease, Parkinson’s disease dementia, olivopontocerebellar atrophy, dementia with Lewy bodies, and Creutzfeldt-Jakob disease can have distinct PET-CT findings allowing early diagnosis. For instance, AD typically demonstrates hypometabolism within a temporoparietal distribution, while FTD demonstrates hypometabolism within the frontal lobes and anterior temporal lobes.
PET-CT is typically used to increase diagnostic accuracy to assist with treatment planning. The diagnostic information offers benefits to patients and families beyond drug treatment decisions. Accurate knowledge of the diagnosis often reduces anxiety and helps families clarify care-giving tasks.
When compared with SPECT imaging, FDG PET-CT offers superior spatial resolution, image quality and accuracy, particularly at early stages of disease, as well as more advanced stages.1
Anatomical imaging (MRI or CT) of the brain is often used to identify unsuspected, clinically significant lesions such as strokes and tumors.
However, in the case of AD, such scans are typically read as normal or misinterpreted as cerebrovascular disease.2
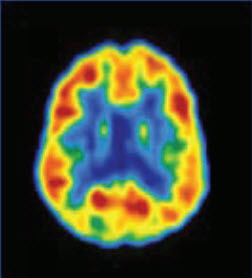
This FDG PET-CT image represents an axial slice through the brain of a normal subject, at the level of inferior parietal/superior temporal cortex. The color displayed in each part of the brain reflects the concentration of the radioactive glucose analog (F-18) fluorodeoxyglucose accumulating at that site, which in turn corresponds to how metabolically active the neurons in that region are. Red, orange, and yellow areas are (in decreasing order) the most active, while green, blue and purple areas are progressively less active. Note, that in neurologically healthy individuals, the entire cerebral cortex has a moderately high level of metabolism.3
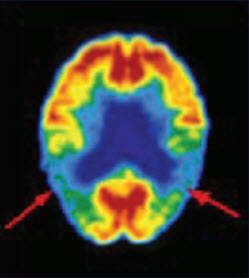
This FDG PET-CT image shows the effects of Alzheimer’s Disease on the activity of the brain. Red, orange, and yellow colors correspond to the relatively high level of metabolism normally present throughout the cerebral cortex. Arrows indicate areas of low activity located in the patient’s parietotemporal cortex, a region important for processing of language and associative memories.3
Medicare and Medicaid Reimbursement for PET-CT
Medicare and Medicaid Services have approved reimbursement for PET in the differential diagnosis of AD and FTD, since the latter does not seem to respond well to symptomatic treatment. Certain criteria are mandated for Medicare reimbursement:
• A recent diagnosis of dementia and documented cognitive decline for more than 6 months
• Presence of diagnostic criteria for both AD and frontotemporal dementia
• Exclusion of alternate neurodegenerative disease or causes
Summary
Alzheimer’s disease is an increasingly important health problem in our aging society. An early differential diagnosis of AD is very critical in making decisions regarding patient treatment and management. Imaging, particularly with PET-CT is the preferred examination to diagnose AD and differentiate it from normal brain function and other neurodegenerative diseases.
PET-CT imaging enables the physician to:
• Detect Alzheimer’s disease accurately at its earliest stage
• Differentiates between Alzheimer’s disease, normal aging, and neuropsychiatric conditions such as depression
• Differentiates between Alzheimer’s disease and other frontotemporal dementias such as dementia with Lewy bodies, Parkinson’s disease and Huntington’s disease
• Determines the likelihood of future deterioration of mental status
1 Messa C, et al. High resolution technetium-99m-HMPAO SPECT in patients with probable Alzheimer’s disease: comparison with fluorine- 18-FDG PET.J Nucl Med. 1994;35:210-216.
2 Coverage request for positron emission tomography (PET) used in the evaluation of Alzheimer’s disease and related dementias. Submitted to CMS on Mary 12, 2003.
3 PetNet Solutions; Alzheimer’s Disease:Positron Emission Tomography:Earlier more accurate detection of Alzheimer’s Disease;alz.fy.08.2004.01.5000©2004